Blood typing is an important aspect of healthcare that involves determining a person’s blood group and Rh factor. Understanding your blood type is crucial in many medical situations, such as blood transfusions or organ transplants, as incompatible blood types can cause serious complications. We will explore the most common blood type in the world and why it’s important to know yours. We’ll also delve into the genetics behind blood typing and how donor and recipient blood types must match for safe transfusions. So whether you’re curious about your own blood type or simply want to learn more, read on for all you need to know.
Blood Typing 101: Understanding the ABO System
Blood typing is the process of determining a person’s blood group and Rh factor. The ABO system is the most important blood typing system used in transfusions and donations.
The ABO system is based on two antigens, A and B, on the surface of red blood cells. There are four main blood types:
A, B, AB, and O.
Type A blood has only the A antigen, type B has only the B antigen, type AB has both, and type O has neither. The presence or absence of these antigens determines a person’s blood type.
In addition to antigens, there are antibodies in the blood that react against the opposite antigen. Type A blood has anti-B antibodies, type B blood has anti-A antibodies, type AB has neither, and type O has both.
Knowing your blood type is important because it impacts your health and medical treatment. Type O negative is a “universal donor” and type AB positive is a “universal recipient”.
The Genetics of Blood Typing: How Your Genes Determine Your Blood Type
Blood typing is determined by the presence or absence of certain antigens on the surface of red blood cells. This is determined by the ABO gene, which has three alleles: A, B, and O.
Each person inherits two alleles, one from each parent. If a person inherits two A alleles, they will have type A blood. If they inherit two B alleles, they will have type B blood. If they inherit one A allele and one B allele, they will have type AB blood. If they inherit two O alleles, they will have type O blood.
The A and B alleles are codominant, meaning they both express their traits equally. The O allele is recessive, meaning it only expresses its trait when paired with another O allele.
Rh factors also determine blood type, with Rh positive and Rh negative determined by the presence or absence of a protein on the surface of red blood cells. This factor is also inherited from parents.
Knowing your blood type is important because it impacts your health and medical treatment. Type O negative is a “universal donor” and type AB positive is a “universal recipient”.
Understanding the genetics of blood typing is important in transfusions and donations to ensure compatibility between donor and recipient. It also helps predict the likelihood of a person’s children inheriting a certain blood type.
Why is Knowing Your Blood Type Important?

Knowing your blood type is essential for several reasons. Firstly, it can impact your health and medical treatment, as well as your ability to donate blood or receive transfusions.
Different blood types have varying antibodies, which can result in complications if given the wrong blood type.
For example, if you have type A blood, you have anti-B antibodies, so you can only receive blood from someone with type A or O blood. On the other hand, if you have type O blood, you can only receive blood from someone with type O blood.
In emergency situations, where there may not be time to test a person’s blood type, type O negative blood is often used because it is a “universal donor” that can be safely given to anyone with any blood type.
Knowing your blood type can also help medical professionals better understand your health risks and tailor treatments accordingly. Certain blood types have been linked to a higher risk of developing certain conditions like heart disease and certain cancers.
The Four Blood Types: A Closer Look at A, B, AB, and O
The four primary blood types are A, B, AB, and O. Each type has unique characteristics determined by the presence or absence of certain antigens and antibodies.
Type A: blood has A antigens on the red blood cell surface and anti-B antibodies in plasma. People with type A can donate to type A and AB individuals, but can only receive from type A and type O.
Type B: blood has B antigens on the red blood cell surface and anti-A antibodies in plasma. People with type B can donate to type B and AB individuals, but can only receive from type B and type O.
Type AB: blood has both A and B antigens on the red blood cell surface and no antibodies in plasma. People with type AB can receive from any blood type, but can only donate to type AB individuals.
Type O: blood has no antigens on the red blood cell surface and both anti-A and anti-B antibodies in plasma. People with type O are “universal donors” who can donate to any blood type but can only receive from type O.
Knowing your blood type can help you better understand your risk for certain medical conditions, such as heart disease and certain cancers, as well as help medical professionals provide appropriate treatments. Additionally, knowing your blood type can be important in emergency situations when blood transfusions may be necessary.
Demystifying Rh Factor: What It Is and Why It Matters for Blood Typing
The Rh factor is another important factor in blood typing that refers to a protein on the surface of red blood cells. It can either be present (Rh+) or absent (Rh-), and knowing your Rh factor is crucial for medical professionals to ensure safe blood transfusions and monitor pregnancies.
If a person is Rh-, they should only receive Rh- blood to avoid an immune reaction. Pregnant women who are Rh- may need Rh immune globulin injections to prevent hemolytic disease of the newborn, where the mother’s antibodies attack the fetus’s red blood cells.
Understanding the Rh factor is important for medical treatment and can have significant implications for pregnancy. Knowing your Rh factor can help prevent potentially dangerous immune reactions and ensure safe medical procedures.
The Most Common Blood Type in the World: Which One Is It?

The most common blood type in the world is O positive (O+), with an estimated 38% of the world’s population having this blood type. The next most common blood type is A positive (A+), with approximately 34% of the population having this blood type.
However, it’s important to keep in mind that the distribution of blood types can vary based on geography, ethnicity, and other factors. For example, in some regions of Africa, the most common blood type is O, while in Japan, the most common blood type is A.
Regardless of your blood type, it’s important to know it for medical treatment and emergency situations. O- blood is considered a universal donor, while AB+ blood is a universal recipient.
In short, while O+ is the most common blood type worldwide, there is still variation depending on location and other factors. Knowing your blood type is important for medical care and emergencies, and understanding the universal donor and recipient types can be helpful as well.
Blood Type Distribution Around the World: Are There Regional Differences?
Blood type distribution varies based on location and ethnicity. In the Americas, the most common blood type is O+, followed closely by A+. In Europe, it’s A+, followed by O+. In Africa, it’s O, followed by A. And in Asia, it’s B+, followed by O+.
It’s also interesting to note that some regions have higher percentages of certain rare blood types. Northern European descent have a higher percentage of the rare blood type AB.
Understanding regional differences in blood type distribution can be important for blood donation and transfusion purposes. Blood banks may need to collect more of certain blood types in areas where they are more prevalent.
While O+ is the most common blood type globally, knowing the regional differences in blood type distribution can be important for medical and donation purposes.
Can Blood Type Affect Your Health or Disease Risk?
Blood type may affect health outcomes. For instance, people with type A blood may have a higher risk of heart disease, while those with type O may have a lower risk. Blood type may also impact susceptibility to infectious diseases, with type O individuals being less susceptible to severe malaria.
In emergency situations, blood type compatibility is crucial for blood transfusions. Knowing your blood type can help you stay informed about your health and disease risk.
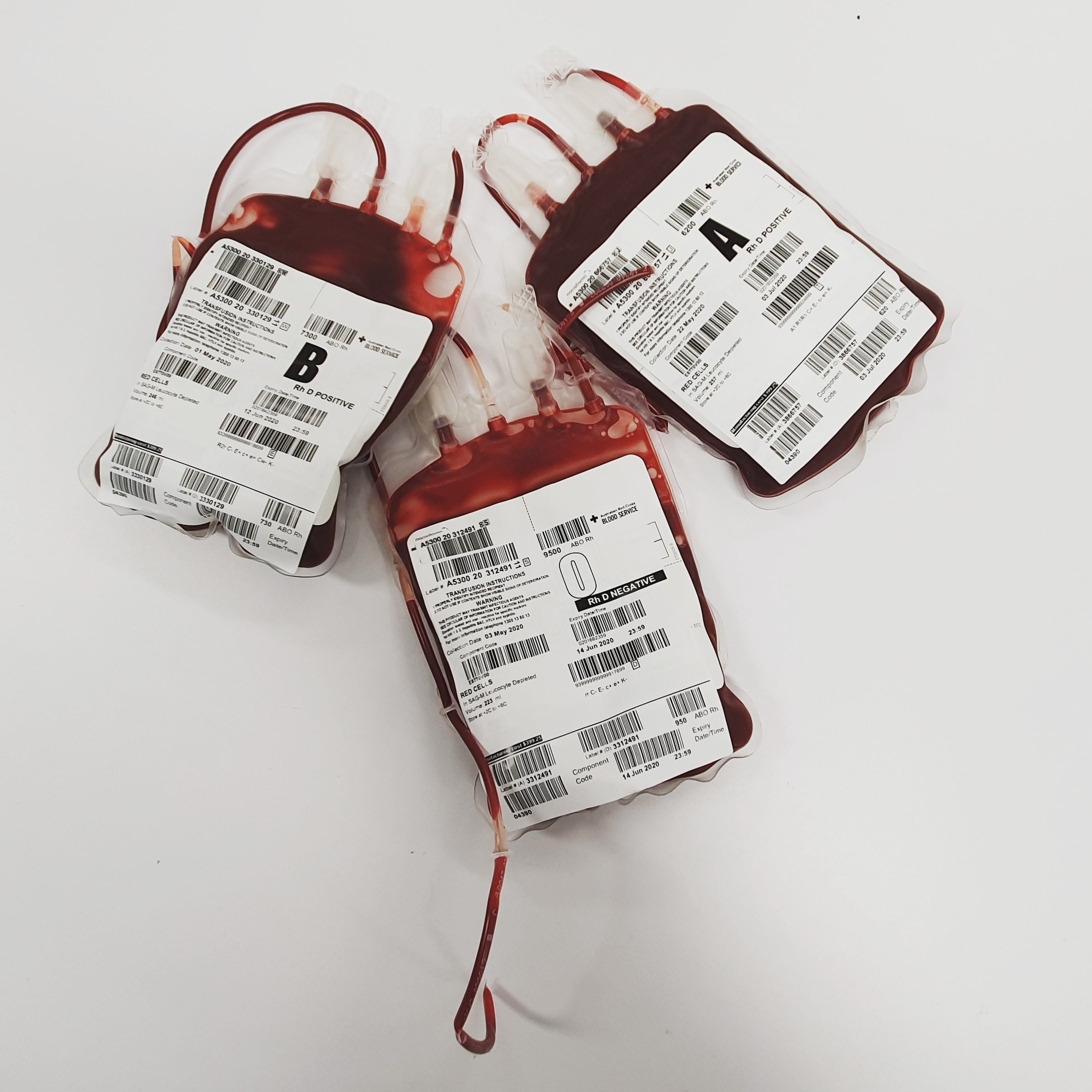
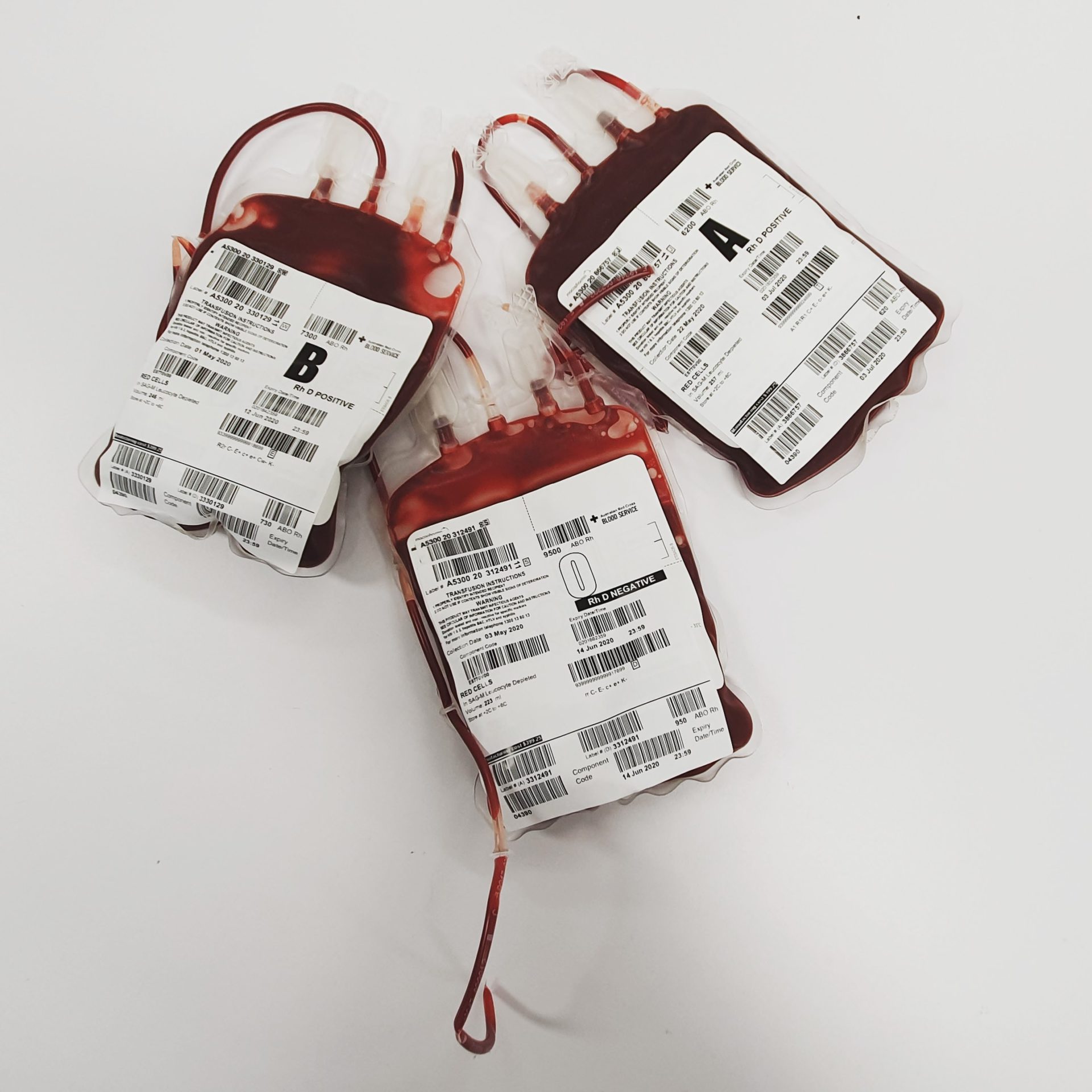
Blood Typing and Transfusions: How Donor and Recipient Blood Types Must Match
Blood transfusions save lives, but it’s important to match the blood types of donors and recipients to prevent complications. The ABO and Rh blood group systems are the most important in transfusion medicine. Type O-negative is the universal donor, and AB-positive is the universal recipient, but transfusions between compatible ABO blood groups can occur. Other blood group systems, such as Kell, Duffy, and Kidd, can also affect transfusion compatibility. Make sure to know your blood type and inform a healthcare provider to ensure safe medical procedures.
The Future of Blood Typing: Advances in Testing and Genetic Engineering

Blood typing and matching have come a long way since their discovery over a century ago. Advances in technology have made testing faster, more accurate, and more widely available.
The development of molecular biology techniques has allowed for the identification of thousands of blood group antigens and their corresponding genes. Scientists are also exploring genetic engineering to create universal blood donors, which would eliminate the need for typing and matching altogether.
Another area of research is the use of synthetic blood substitutes, which could provide a safe and readily available alternative to donated blood. While there is still much to learn about blood typing and transfusion medicine, ongoing research and innovation continue to improve patient outcomes and save lives.