Heart disease doesn’t usually begin with chest pain or a dramatic ER visit. It starts quietly years, sometimes decades earlier deep inside your metabolism. The real culprit behind many heart attacks isn’t just cholesterol. It’s insulin resistance. And most people never hear about it until it’s too late.
Let’s talk about the blood markers that actually connect insulin resistance to heart disease and why they’re often ignored.
What is Insulin Resistance?
Insulin resistance happens when cells in your muscles, fat and liver don’t respond to insulin as they should. This is also known as impaired insulin sensitivity. Insulin is essential for life and regulating blood glucose (sugar) levels.
Insulin helps move glucose from your blood into your cells so your body can use it for energy. For several reasons, your cells can respond inappropriately to insulin. This means they can’t efficiently use the glucose for energy or for storage. As a result, glucose continues to build up in your blood. Your pancreas makes more insulin to try to overcome your increasing blood glucose levels. This is called hyperinsulinemia.
As long as your pancreas can make enough insulin to balance out your blood sugar levels, they’ll stay in a healthy range. If your cells become too resistant to insulin, it leads to elevated blood glucose levels (hyperglycemia).
Over time, hyperglycemia can lead to prediabetes and Type 2 diabetes.
The condition is also associated with:
- Obesity
- Cardiovascular disease
- Metabolic dysfunction-associated steatotic liver disease
- Metabolic syndrome
- Polycystic ovary syndrome (PCOS)
Why Insulin Resistance Is the Silent Driver of Heart Disease?
Insulin resistance is like a jammed lock. Your body keeps producing insulin, but your cells stop responding properly. Sugar stays in the bloodstream. Insulin levels rise. Fat metabolism shifts. Inflammation creeps in.
Long before blood sugar crosses the diabetes line, insulin resistance is already damaging arteries. By the time someone is diagnosed with heart disease, the metabolic dysfunction has usually been there for years.
What Metabolic Syndrome Really Means?
Metabolic syndrome isn’t a disease it’s a warning system. It’s a cluster of conditions that travel together:
Elevated triglycerides
Low HDL cholesterol
High blood pressure
Abdominal fat
Elevated fasting glucose
Behind all of them? Insulin resistance.
Why Heart Disease Starts Years Before Symptoms
Arteries don’t clog overnight. Plaque forms gradually, driven by insulin-driven inflammation, abnormal lipid particles, and endothelial damage. Waiting for symptoms is like waiting for smoke when the house has been burning for years.
The Link Between Insulin Resistance and Heart Disease
When you think about heart disease, the usual suspects probably come to mind: high blood pressure, cholesterol, maybe smoking or lack of exercise. But insulin resistance often slips under the radar, even though it’s one of the most powerful drivers of cardiovascular dysfunction.
Here’s how it works: insulin resistance leads to chronic inflammation, increased oxidative stress, and damage to the endothelium — the delicate lining of your blood vessels. Over time, this damage promotes plaque buildup (atherosclerosis), narrows your arteries, and increases the risk of blood clots and heart attacks.
But that’s not all. Insulin resistance also throws your lipid profile out of whack. It contributes to higher triglycerides, lower HDL (the “good” cholesterol), and increased levels of small, dense LDL particles — which are more likely to penetrate arterial walls and cause blockages.
This is the hidden metabolic storm brewing beneath the surface.
So even if your cholesterol numbers look fine on paper, insulin resistance may be silently degrading your cardiovascular health. By the time your doctor detects heart disease, insulin resistance has likely been at work for years — if not decades. That’s why it’s crucial to go beyond traditional cholesterol panels and dig deeper into what your metabolism is really doing.
Insulin Resistance Blood Tests That Matter
Fasting Insulin: The Missing Metric
Fasting insulin is one of the earliest indicators of metabolic dysfunction. Elevated insulin often appears years before glucose abnormalities. Yet it’s rarely ordered.
Optimal fasting insulin is low—not just within lab range.
Triglycerides: More Than a Fat Marker
Triglycerides rise when insulin can’t properly manage energy storage. Elevated triglycerides are one of the strongest signals of insulin resistance and future cardiovascular events.
ApoB: The Particle Count That Predicts Events
ApoB represents the number of atherogenic lipoproteins circulating in your blood. Each particle is a potential plaque starter. High ApoB equals higher risk—regardless of LDL-C.
LP-IR Score: Early Detection Before Diabetes
The LP-IR score integrates lipoprotein patterns to estimate insulin resistance. It’s especially powerful for identifying risk in people who appear metabolically “normal.”
Why High Triglycerides Signal Insulin Dysfunction?
When insulin resistance develops, the liver overproduces triglyceride-rich particles. This shifts LDL into smaller, denser forms that penetrate arterial walls more easily.
ApoB and Atherosclerosis Progression
ApoB tells you how many of those particles are circulating. High triglycerides plus high ApoB is like speeding traffic on icy roads—plaque formation accelerates.
How Insulin Resistance Damages the Heart?
Endothelial Dysfunction
Insulin resistance impairs nitric oxide production, reducing blood vessel flexibility. Arteries become stiff, raising blood pressure and injury risk.
Chronic Inflammation and Plaque Formation
Elevated insulin promotes inflammatory signaling. Inflammation destabilizes plaque, increasing the risk of rupture and heart attack.
Small Dense LDL Particles
Insulin resistance favors small dense LDL particles, which are more likely to oxidize and embed in arterial walls.
Why These Markers Are Often Missed?
Insurance-Driven Testing Models
Most healthcare systems focus on disease diagnosis, not early risk. If you’re not diabetic or post-heart attack, advanced markers are often skipped.
Reactive vs Preventive Medicine
The system is designed to treat fires, not smoke. Preventive testing challenges that model.
Who Should Be Tested for Insulin Resistance
Normal Weight, High Risk
You don’t need obesity to have insulin resistance. Genetics, stress, sleep deprivation, and sedentary behavior all play a role.
Family History and Hidden Genetics
A family history of heart disease, diabetes, or stroke dramatically raises risk—even with “normal” labs.
Who Does Insulin Resistance Affect?
Insulin resistance can affect anyone — you don’t have to have diabetes — and it can be temporary (for example, using steroid medication for a brief period causes insulin resistance) or chronic. The two main factors that seem to contribute to insulin resistance are excess body fat, especially around your belly, and a lack of physical activity.
Having a family history of insulin resistance (family members with prediabetes, type 2 diabetes, and/or PCOS) can also contribute to insulin resistance.
People who have prediabetes and Type 2 diabetes usually have insulin resistance. People with Type 1 diabetes can also experience insulin resistance.
What Are The Symptoms of Insulin Resistance?
If you have insulin resistance, but your pancreas can increase insulin production to keep your blood sugar levels in range, you won’t have any symptoms.
But over time, the condition can get worse, and the cells in your pancreas that make insulin can wear out. Eventually, your pancreas can’t produce enough insulin to overcome it, leading to elevated blood sugar.
People with consistently high blood sugar levels can experience the following symptoms:
- Unexplained weight loss
- Fatigue
- Increased thirst
- Frequent urination (peeing)
- Increased hunger
- Blurred vision
- Yeast infections
Many people have no symptoms of prediabetes, often for years. Prediabetes may be invisible until it develops into Type 2 diabetes. Some people with prediabetes may experience the following symptoms:
- Darkened skin in your armpit or back and sides of your neck, called acanthosis nigricans
- Skin tags
- Eye changes that can lead to diabetes-related retinopathy
If you’re experiencing any of these symptoms, it’s important to see your healthcare provider.
What Causes Insulin Resistance?
Scientists still have a lot to discover about how exactly it develops. So far, they’ve identified several genes that make a person more or less likely to develop insulin resistance. Providers also know that gaining weight can worsen it, and losing weight can help improve it. Other factors and conditions can cause varying degrees of the condition.
Acquired causes of insulin resistance
Acquired causes of the condition, meaning you’re not born with the cause, include:
- Excess body fat: Scientists believe obesity is a primary cause of insulin resistance. Excess fat in your belly and around your organs (visceral fat) especially raises your risk.
- Physical inactivity: Movement and exercise make your body more sensitive to insulin. Exercise also builds muscle that can absorb blood glucose. A lack of physical activity can lead to the condition.
- Food choices: A diet of highly processed foods, high in carbohydrates and saturated fats, has been linked to the condition
- Certain medications: Steroids, blood pressure medications, HIV treatments and other medications can cause insulin resistance.
Hormonal disorders that can cause insulin resistance
Issues with certain hormones can affect how well your body uses insulin. Hormonal disorders that can cause insulin resistance include:
- Cushing’s syndrome: This rare condition happens when there’s extra cortisol in your body. Excess cortisol can counteract the effects of insulin, causing the condition.
- Acromegaly: This is a very rare but serious condition that happens when you have high levels of growth hormone (GH). High levels of GH can lead to insulin resistance.
- Hypothyroidism: This means your thyroid is underactive and doesn’t produce enough thyroid hormone. It causes your metabolism to slow down, which can lead to insulin resistance.
Genetic conditions that cause insulin resistance
Certain inherited genetic disorders — conditions you’re born with – can cause the condition for various reasons. These are rare but include Type A insulin resistance syndrome and Donohue syndrome.
Other inherited conditions that can cause it include:
- Myotonic dystrophy: This is a form of muscular dystrophy that affects your muscles, eyes and endocrine system organs.
- Alström syndrome: This condition causes obesity and Type 2 diabetes. It also causes vision and hearing loss, dilated cardiomyopathy and short stature.
- Werner syndrome: A condition that causes accelerated aging (progeria). It affects many aspects of your body, including resistance to the effects of insulin.
- Inherited lipodystrophy: This is a condition in which your body doesn’t use and store fat properly.
How Is Insulin Resistance Diagnosed?
Insulin resistance is difficult to diagnose because there isn’t routine testing for it. As long as your pancreas is producing enough insulin to overcome the resistance, you won’t have any symptoms.
Your healthcare provider will consider several factors when evaluating you for the condition. These might include your:
- Medical history
- Family history
- Physical exam
- Signs and symptoms
What Tests Will Be Done to Evaluate Insulin Resistance?
Your healthcare provider may order the following blood tests to diagnose the condition:
- Glucose test. A fasting plasma glucose (FPG) or a blood glucose test can screen for prediabetes, type 2 diabetes or gestational diabetes.
- A1c test. This test reveals your average blood glucose levels over the past three months.
- Lipid panel. This is a group of tests that measure specific lipids in your blood.
How is Insulin Resistance Treated?
Not all factors that contribute to the condition can be treated, such as genetic factors and age. For this reason, lifestyle modifications are the primary treatment for insulin resistance. Lifestyle modifications include:
- Eating nutritious foods. Your healthcare provider may recommend reducing carbohydrates and unhealthy fats. That might mean eating less sugar, red meats and processed starches. Instead, they’ll likely recommend eating more whole foods, like vegetables, fruits and whole grains. For protein, they might suggest more fish and lean poultry.
- Physical activity. Getting regular amounts of moderate-intensity physical activity can help. It helps increase glucose energy usage and improves muscle insulin sensitivity.
- Losing excess weight. In some cases, losing weight can improve insulin resistance. Your healthcare provider can suggest strategies for weight loss.
Over time, these lifestyle modifications can:
- Reduce insulin resistance
- Lower your blood glucose levels
- Decrease blood pressure
- Decrease triglyceride and LDL (“bad”) cholesterol levels
- Raise HDL (“good”) cholesterol levels
Your healthcare provider might refer you to a specialist, like a dietitian or endocrinologist. They’ll work together with you to come up with an individualized treatment plan.
What Medications Are Used to Treat Insulin Resistance?
There are currently no medications that treat the condition specifically. Your healthcare provider may prescribe medications to treat coexisting conditions. Some examples include:
- Blood pressure medication
- Metformin for diabetes or prediabetes
- Statins to lower LDL cholesterol
Can I Reverse Insulin Resistance?
The condition has several causes and contributing factors, and not all causes are reversible. But lifestyle changes can make a difference. Eating nutritious foods, exercising regularly and losing excess weight may decrease your insulin resistance. Talk to your healthcare provider about what you can do to best manage it.
How Can Diet Affect Insulin Resistance?
What you eat can have a big impact on your blood sugar and insulin levels. The glycemic index (GI) is a tool that can help you determine what foods have the biggest impact on your blood sugar levels.
High-GI foods generally have a lot of carbohydrates and/or sugar. They cause your blood sugar to increase quickly and require a lot of insulin to bring blood sugar back down. You’ll want to avoid high-sugar drinks like regular soda and juices, and avoid eating excess amounts of the following foods:
- White bread
- Potatoes
- Breakfast cereals
- Cakes and cookies
- Fruits such as watermelon and dates
Low-GI foods cause a steadier rise in blood sugar. Your pancreas doesn’t have to work as hard to release insulin. Eating foods that are lower on the glycemic index is generally better for people with insulin resistance:
- Beans and legumes
- Fruits such as apples and berries
- Non-starchy vegetables, such as asparagus, cauliflower and leafy greens
- Nuts
- Dairy, fish and meat
Always talk to your healthcare provider before making extreme changes to your eating patterns.
Preventive Testing: What to Ask Your Doctor For
So, what can you do about all this?
Step one: start testing the right markers.
Here’s a list of blood tests you should request even if your doctor doesn’t bring them up:
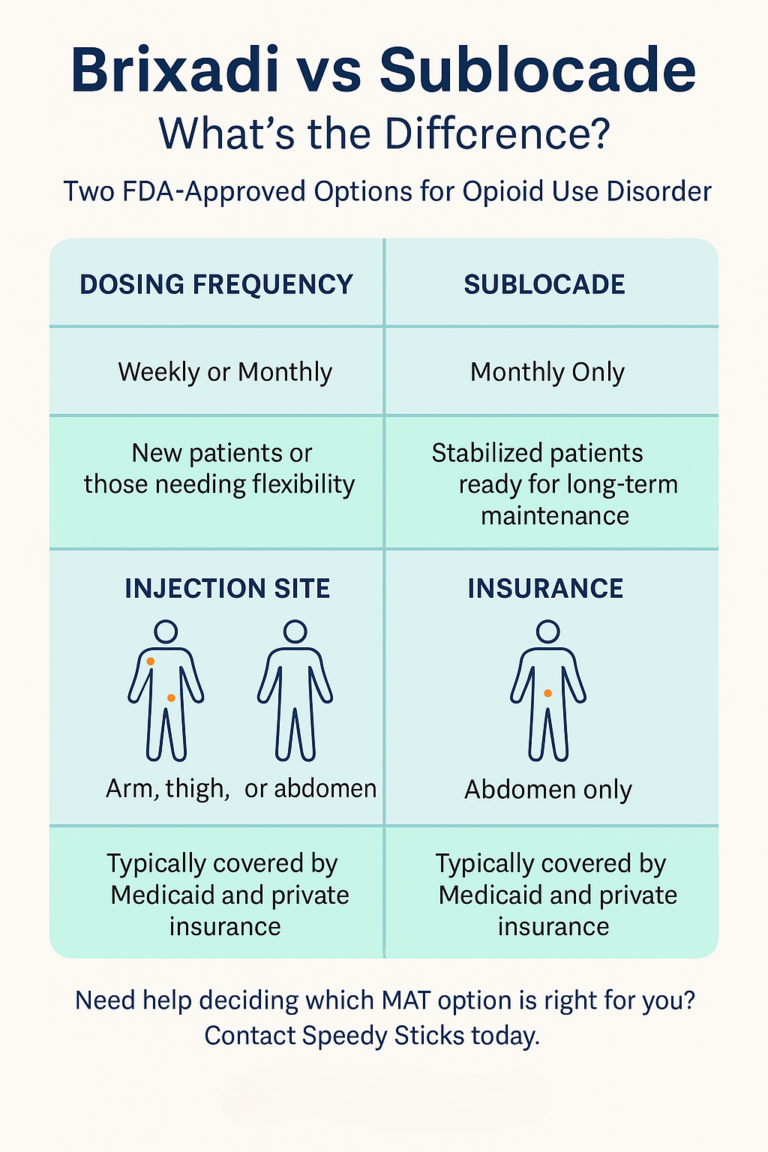
| Test | Why It Matters | Optimal Range |
|---|---|---|
| Fasting Insulin | Early marker of insulin resistance | 2–6 µIU/mL |
| Triglycerides | Reflects liver and carb metabolism | <100 mg/dL |
| HDL Cholesterol | Protective against heart disease | >60 mg/dL |
| Triglyceride-to-HDL Ratio | Strong IR predictor | <2:1 |
| ApoB | Best marker of atherogenic particles | <80 mg/dL |
| LP-IR Score | Lipid-based IR assessment | <45 |
| hs-CRP | Measures systemic inflammation | <1.0 mg/L |
| Fasting Glucose | Basic but limited | <90 mg/dL |
| HbA1c | Average 3-month glucose | <5.3% |
Ask your doctor specifically for these and if they push back, consider working with a functional medicine provider who understands the importance of early detection.
You only get one heart. Don’t leave its fate up to chance.
Speedy Sticks and the Future of Preventive Blood Testing
Let’s face it the healthcare system is built more for reaction than prevention.
That’s where companies like Speedy Sticks come in. Instead of waiting for disease to strike and then scrambling to treat it, Speedy Sticks helps people get ahead of the game with at-home, personalized blood testing.
Think of it as your preventive health concierge. You choose the tests you want (like fasting insulin, ApoB, LP-IR, or hs-CRP), schedule a quick visit, and get your results — without ever stepping foot into a doctor’s office.
The benefits?
Convenience: No waiting rooms, no lost time
Clarity: You get access to the markers that matter
Control: You decide what to test and when
Conclusion
Insulin resistance is the metabolic bridge between everyday lifestyle and heart disease. It doesn’t announce itself loudly, but it leaves clues in the blood—fasting insulin, triglycerides, ApoB, and LP-IR. Ignoring these markers means reacting to disease instead of preventing it. The future of heart health isn’t about waiting for symptoms. It’s about seeing risk early and acting before damage is done.
The blood markers we covered — fasting insulin, triglycerides, ApoB, LP-IR, and more — are powerful tools that can uncover hidden risks years before traditional tests pick them up. Don’t let outdated lab panels be the reason you miss your warning signs.
Take control. Get tested. Know your numbers. And if your doctor won’t run the labs, take matters into your own hands with services like Speedy Sticks. Prevention isn’t just smart — it’s life-saving.
Speedy Sticks bridges the gap between data and action, giving you insights your typical primary care visit might miss. It empowers you to make better decisions before problems become crises.
Speedy Sticks offers licensed, at-home blood draws for advanced cardiovascular testing, including ApoB and lipid panels.
✔ Nationwide coverage
✔ Professional phlebotomists
✔ Convenient, compliant collections
Book an at-home blood draw today
Say Goodbye To Waiting Rooms And Long Lines. Speedy Sticks offers at-home testing.